
Burning Mouth Syndrome (BMS)
Burning Mouth Syndrome (BMS) is described as a burning sensation in the tongue or other sites in the oral cavity. It is usually idiopathic with no clinical or laboratory findings. As well as the burning or scalding sensation to the tongue or palate, symptoms may include: lack of saliva, changes to the tongue mucosa, altered taste (metallic, bitter) and temporomandibular joint pain. This condition is relatively common, with the estimated prevalence in recent studies ranging from 0.7 to 4.6% of the general population. There is speculation that the hormonal changes of menopause may be a factor with this condition, because of the high incidence in middle- aged women.
Standard treatment of BMS is usually pharmaceutical with drugs including benzodiazepines, tricyclic antidepressants, anticonvulsants, alpha-lipoic acid, and topical capsaicin.
This is a review of 22 case studies of Burning Mouth Syndrome thatI have treated clinically in the last few years.
Etiology
The cause for BMS given by these patients include the following: a sudden onset from spicy food (1), insidious (10), dental work (filling replaced) (3), ill fitting night guard (1), post turbinate surgery (1), extensive facial surgery (post MVA) (1) facial fractures (3), bitten tongue,(1) post wisdom teeth extraction severed lingual nerve (1), and facial shingles with extensive scarring (1), .
After taking a thorough history of these patients, I found that there were multiple previous dental or cranial injuries, surgeries and pathologies that I believe all had a role to play in their BMS. I believe that multiple scarring around the cranial nerves, from different traumas or conditions result in BMS. That may be why it appears in the menopausal age group and in women tend, who have had more dental work or facial procedures than men.
1. Suspected Anatomical Causes
I have documented from their medical history what I believe had a role in their BMS symptoms.
2. Pterygopalantine Ganglion Impingement
Scarring or pressure on the pterygopalantine ganglion was present in nearly all of the subjects with nearly half having had impacted wisdom teeth extracted or major work done on the back teeth. This ganglion may be paramount in the diagnosis and treatment of BMS. The pterygopalantine fossa gets reduced with prolonged mouth opening or when wisdom teeth are pulled and the fossa gets closed.
Â
 Scar tissue or irritation of the following sites on the cranial nerves
- Trigeminal nerve – Maxillary nerve portion
- superior alveolar nerve plexus with tooth implants
- dental and gingival branches from caps and braces
- middle superior alveolar nerve from cheek implants (titanium) and fillers with cosmetic work
- anterior superior alveolar nerve from nose reconstruction and deviated septum
- pterygopalantine ganglion entrapment post wisdom teeth removal, prolonged jaw opening, post intubation and prolonged dental work
- complications of amalgam replacement – potential reaction of composite materials
- severe sinus problems
- polyps surgery
- braces on back of front teeth
- cheek lift surgery
- ill fitting night splint can irritate the nerves on the roof of the mouth
- post surgical malalignment after facial reconstruction
- Trigeminal nerve -Ophthalmic nerve portion
- external nasal branch of the anterior ethmoidal nerve from deviated septum repair or nasal surgery
- supraorbital nerve from extensive scarring from facial shingles
- eye surgery post facial reconstruction (MVA)
- severe eye infection
- Trigeminal nerve -Mandibular nerve portion
- sublingual nerve from biting the tongue
- sublingual nerve severed during wisdom teeth extraction
- submandibular gland dysfunction from calcium deposits and mumps
- sublingual gland damage
- buccal nerve damage following facial reconstruction
- cyst removal on side of face
- cheek lift
- tongue ulcers
- a lot of dental work as child, 10 crowns over last 5 years
- trigeminal meralgia before BMS
- TMJ dysfunction causing problems with the otic ganglion that serves the lingual nerve
- Infections (dry socket) post tooth extraction
- Optic nerve
- eye surgery and facial reconstruction
- Vestibulocochlear nerve
- severe ear infections
- tinnitus
- Glossopharyngeal nerve
- Tonsils removed
- Ulcers on posterior aspect of the tongue
- Parotid gland calcifications
- Facial Nerve
- Facial reconstruction post MVA
- Hypoglossal Nerve
- Bitten tongue
- Mumps
- Intubation post surgeries
- Growth on vocal cords
- Nasal nerves
- Superior posterior lateral nasal branches from pterygopalantine ganglion- submucosal
- reduction on turbinates using cold laser surgery
- Septum repairs
3. Mechanical causes
TMJ
Half of the patients had temporomandibular dysfunction and pain with clicking from displaced discs, bruxism, or joint dysfunction (hyper or hypomobility). This dysfunction can lead to problems with the otic ganglion which feeds the lingual nerve.
4. Head And Facial Injuries
5. Submandibular Duct or Gland
Blockage of the duct with calcium or problems with the gland seem to occur in several of the subjects with dry mouth and lack of saliva
Common Problems in the Subjects
The most common problem with the case studies were compromises of the pterygopalantine ganglion from wisdom teeth removal (13), cervical spine pathology (16), TMJ dysfunction (14), surgeries with intubation (14), sinus problems (11), root canals (8), a lot of crowns (8), salivary gland dysfunction (6), tongue bitten or injured (3), tonsillectomy (4), a lot of cavities as a child (5), mumps (2), parotid gland dysfunction (1), reflux (3), facial shingles (1), braces (5), deviated septum surgery (2), ear infections and tubes (2), hearing loss (2), head injury or concussion (3), submandibular gland dysfunction (2), cyst on face (1) , cheek lift (1), growth on vocal cords, braces or retainer (4), ear surgery (1), turbinate surgery (1), facial scarring (2), and tinnitus or vertigo (5).
It was interesting to note how many facial, TMJ, dental and cervical pathologies were present in these subjects.
The pterygopalantine ganglion has branches that serve the greater and lesser palantine nerves. If it is compressed in the sphenopalantine fossa, it will create sensory changes to the roof of the mouth or maxilla. It can be compromised with prolonged jaw opening, dental surgery (wisdom teeth extraction), intubation or extensive dental work. The lateral plates of the pterygoid process compress the ganglion with the jaw forced open or held open too long.
Common Complaints
Burning of the tongue and/or upper palate (13)
Burning of just the tongue (4)
Burning of just the upper palate (4)
Back of tongue and throat (2)
Burning of lip as well (4)
Mouth and lip dryness, lack of saliva, Sjogern’s syndrome (9)
Pain level 3-8 (7) 6-10 (9) 1-5 (1)
Sinus problems (11)
Red rash on tongue (2)
White coating on tongue (3)
Salt and metallic taste (7)
Ulcers on tongue (2,)
Awake with no burning but burning increases as the day goes by (20)
Acid Reflux (5)
Aggrevating Factors
Talking (9)
Spicy food (3)
Bitter or food high in acidity (5)
Alcohol (1)
Regular toothpaste (5)
Stress (15)
Relieving Factors
Sleeping (10)
Eating or chewing (15)
Hot food (2)
Cold Water (2)
Exercise (2)
Mental visualizations (2)
Treatment
I used manual and osteopathic techniques on the cervical spine, cranium and intraoral structures.
In most cases, I started at the cervical spine with a suboccipital release and cervical traction and mobilization as needed. I found that the suboccipital region tended to be very tight maybe because of the shared innervation from the cervical plexus.
I also worked on the fascia that I found tight including: the geniohyoid fascia, superficial, middle and deep cervical fascia. The often found myofascial trigger points in the following muscles: sternocleidomastoid, temporalis, masseter, and trapezius. Manual techniques were done on the trigger points.
Once I had freed the soft tissue around the neck and jaw, I would go to the temporomandibular joint. After assessing the joint bilaterally, I would gently mobilize both joints. I would work on the capsular ligaments, the stylomandibular ligament, the sphenomandibular ligament, and the lateral temporomandibular ligament. I often found hypomobility unilaterally or bilaterally, a displaced articular disc or joint crepitus.
On all patients I would open up the pterygopalantine canal with an intraoral technique to free up the pterygopalantine ganglion. One patient had complete relief from their BMS with this technique alone. With gentle pressure behind the wisdom teeth, on the hamulus of the plates of the ptergoid process the pterygopalantine fossa can be opened. I found that on the majority of the patients one or both of these fossa were very tight and painful. The normal tissue feels hard but has give to it. The fossa that are closed have a very rigid and hard feeling on the hamulus and usually more painful on the blocked side. I believe that this ganglion and fossa are often compromised with wisdom teeth extraction, intubation or prolonged dental work.
Intraorally, I would work on the submandibular and sublingual glands. On some patients I would feel a granular texture to the gland especially if the gland had been compromised with calcium deposits, mumps, mononucleosis or repeated mouth infections or ulcers. I would trace the salivary ducts intraorally and again often found scar tissue, granules or tightness in the patients that had reduced saliva or Sjogerns syndrome. One patient had saliva flow increase dramatically at the end of the first session.
I would work on the cranial lesions that I found due to head trauma, dental work or surgical procedures. Common findings were sinus restrictions, facial trauma, facial surgery and dental work (tooth extraction, implants, root canals, braces and maxillar retainers).
At the end of treatment, I would work on the involved nerves that I felt were compromised or entrapped. By using eye movements for the optic nerves, temporal bone rotation for the vestibulocochlear, and the tongue for the trigeminal nerve, I would try to free up the restrictions. I would finish by actually tractioning the tongue to floss the whole length of the trigeminal nerve.
Each patient had different reasons for their BMS so each had a slightly different manual approach.
Just like sciatic pain comes from spinal conditions, I believe that burning tongue is just the result of restrictions in the cranial nerves as listed above. I also feel that it appears in women more than men since they generally have had more corrective work done on their teeth and cosmetic surgery over the years. I found that the 2 men in the study were the exception with one having had the nerve severed and the other with the pterygopalantine ganglion entrapped. In all the women patients, there were several nerve entrapments in different areas in the cranium. The accumulation of entrapments throughout the skull eventually causes changes o the trigeminal nerve to the maxilla and/or mandible. Because the lingual nerve to the tongue is the most distal and the most active part of the neural change it sets up as burning mouth. Just like cervical dysfunctions can cause carpal tunnel.
Results
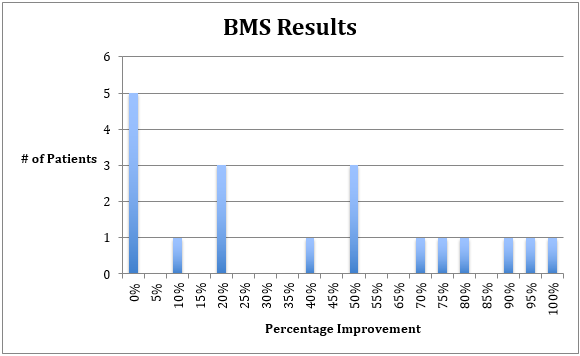
I was only able to reach 19 of the 22 patients for the results. Five patients showed no improvement from the treatment. I recorded below the reasons why they may not have improved. Five patients showed between a 10-40% improvement. Three had a 50% improvement. Five had between 50 and 95 % improvement and one was 100%. Please see the chart below.
Â
Mechanical Problem
I believe there are mechanical problems which affects the cranial nerves, because with rest BMS settles down. The majority of patients felt the symptoms were the least in the morning and got worse as the day progressed. The more they spoke, the more their burning which could indicate that the mechanical tension from using the tongue and pulling on the mandibular part of the trigeminal nerve and into the rest of the cranial nerve connections
Secondly, I found adhesions and restrictions along the pathways of the traumatized nerves which responded with treatment. Opening the pterygopalantine ganglion, mobilizing the submandibular gland, tractioning the lingual nerve all helped change their symptoms.
All of these patients had a lot of neural compromise when I took their history and did the assessment. Most patients had at least 8 different restrictions to the nerves, soft tissue or surrounding joints. Most of these patients have significant cervical spine pathology.
Lack of Improvement
I believe some did not get improvement because I did not have enough visits with them. Five only came for one visit. The most improved patients averaged 4 – 5 sessions. Considering the nature of the condition, the number of restrictions and longevity of the condition in the patients, a number of sessions are necessary. One patient that came for 5 sessions but did not improve I believe had a reaction to the dental amalgam and did not fit as a typical BMS.
Â
Improvement then it Returned
Some people improved after the first couple of days then regressed. I believe that happened because I did not clear all the causes. When I first started to treat this problem I was not aware of all the different neural restrictions. Time taught me how to treat more effectively. My results are better now then when I started. Â Most patients still have some pain that fluctuates with stress.